HARARE, July 20, 2019 (BSS/AFP) – Blessing Chingwaru could barely walk
without support when he arrived at the specialist Rutsanana clinic in Harare
complaining of chest pains and fatigue.
Weighing a skeletal 37 kilogrammes (5.8 stone), the HIV-positive motor
mechanic knew something was wrong.
He was immediately given a number of tests and told the bad news: He was
also suffering from advanced-stage tuberculosis. Dual infection by HIV and TB
is a notorious killer.
“My health was deteriorating and I kept wondering why,” Chingwaru, 29,
recalled at the clinic.
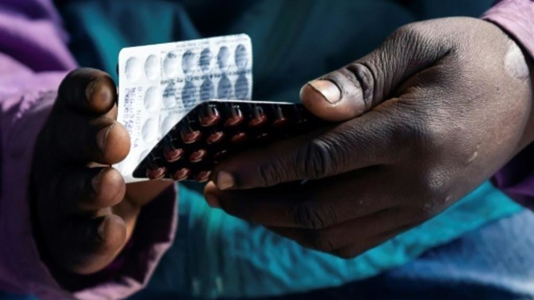
Within hours of the diagnosis, Chingwaru was given free treatment and
nursing care.
In a country where more than a dozen people die each day from TB-related
sicknesses, it was a rare example of efficient public healthcare.
The Rutsanana Polyclinic in Harare’s poor suburb of Glen Norah, which
Chingwaru visited, is one of 10 pilot clinics in the country offering free
diagnosis and treatment for TB, diabetes and HIV.
The clinic, which opened in 2016, is staffed by 24 nurses and currently
treats 120 TB patients.
Among the million-plus people living with HIV in Zimbabwe, TB is the most
common cause of death, according to the World Health Organization (WHO).
HIV-positive people, and others with weakened immune systems, are
particularly vulnerable to contracting the infection.
After Chingwaru’s initial visit in February, doctors had feared for his
life.
But following five months of careful treatment Chingwaru has gained 15
kilos.
“Everything I need, I get here,” said Chingwaru, forming fists with both
hands to show off his regained strength.
– Economic and financial crisis –
In a country where public health services have practically collapsed,
containing the spread of TB has been a persistent struggle.
Zimbabwe has been stuck in a catastrophic economic and financial crisis for
decades and its doctors are underpaid and under-equipped.
Although TB treatment is free, the annual number of TB infections in
Zimbabwe remains among the highest in the world.
The contagious infection is usually found in the lungs and is caught by
breathing in the bacteria from tiny droplets sneezed or coughed out.
As HIV-positive people are so vulnerable to TB, the clinics have followed
the advice of WHO officials to link TB testing and treatment with HIV
prevention programs.
– ‘Catastrophic costs’ –
Close to the main gate of the Rutsanana clinic, a green self-testing HIV
tent has been erected to encourage people to check their status.
The clinic also offers voluntary HIV counselling and antiretroviral
treatment.
Sithabiso Dube, a doctor with the medical charity International Union
Against TB who heads the TB and HIV programme, said people with diabetes also
have a higher risk of developing TB, so patients are tested for both
diseases.
“Instead of going to seek diabetic care at one clinic and TB care at
another, they are able to get these services in one place,” Dube told AFP.
Because services are free “they are able to cut down on what we call
catastrophic costs to the TB patients,” she said.
Largely funded by a US Agency for International Development (USAID)
programme, the pilot clinics have become lifesavers for the poor — but only
if they happen to live near them.
The vast majority of the population have no access to the one-stop clinics.
As a result there are plans to scale up the programme, with another 46
similar centres to be rolled out across Zimbabwe.
Rutsanana clinic matron Angela Chikondo said the programme was crucial to
minimising complications among TB and diabetes patients.
“If one is on TB treatment and also has diabetes, and the diabetes is well
controlled, chances of recovering are very high,” she said.